Receding gums and periodontitis are leading causes of tooth loss in the US. Between 30% and 50% of the population are at risk of developing some form of gum disease. This article will attempt to clarify the causes and effects of receding gums, while also underlining a number of treatments and prevention methods.
Gum disease can be very dangerous. Left untreated, it can lead to complete tooth loss and even worse complications. However, modern treatment and prevention methods can successfully combat receding gums.
Receding Gums – Causes
In most cases receding gums are a symptom of periodontitis. Periodontitis is a general term for a set of bacterial diseases. They cause gum infection, receding gums and, eventually, tooth loss. Worse, untreated gum disease can expose you to heart illnesses and other dangerous medical conditions.
The mechanism of the disease is simple, yet difficult to counter without seeking professional help from a dentist. In many cases, early symptoms are inconspicuous. The disease is thus often ignored until later stages when treatment becomes more difficult.
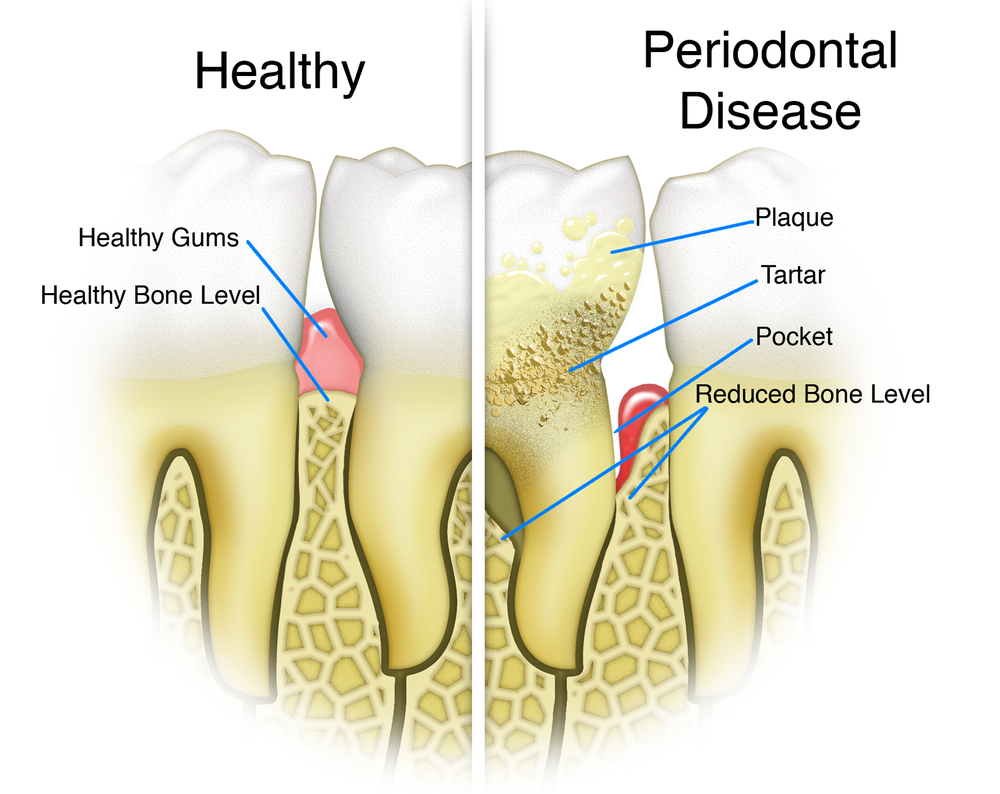
The main trigger of periodontitis is poor oral hygiene, which allows bacteria to accumulate at the base of the teeth. Sometimes, bacteria might even start to build underneath your gums. As the bacteria multiplies, plaque, or biofilm, starts to build up at the base of your teeth. The plaque is extremely resilient to brushing. However, you can prevent its growth by maintaining a strict daily oral hygiene.
Receding Gums – Stages
The Gingivitis Stage
In case of sub-optimal oral hygiene, plaque continues to grow at the base of your teeth until bacteria begin to infect the surrounding gum tissue. This stage is generally known as gingivitis. Depending on the person’s immune system and overall health, the disease might not progress to periodontitis for a long time.
The immune system attempts to combat the bacteria. However, due to the external source of the infection (the plaque on your teeth, which is outside the circulatory system), the body’s defenses cannot reach the source.
If you do nothing at this stage, and if other medical conditions create a favorable environment, the body will react by increasing inflammation in order to combat the infection. This usually leads to gum bleeding, which creates an even more favorable environment for bacteria.
The Periodontitis Stage
Due to constant inflammation, the gum line begins to recede, revealing tooth roots and, eventually, bone. This progresses slowly over time but, in the end, it can cause irreparable damage to your soft and bone tissue and can lead to further complications. Treatment at this stage is possible, but ideally, you should prevent periodontitis early on.
Receding Gums – What are the Symptoms?
The main symptoms of periodontitis are as follows:
- Bleeding and/or dark red gums. This points out that the gums are fighting infection. This symptom may occur during gingivitis and before the disease has significantly progressed. As such, seeking treatment immediately after you notice gum bleeding is the wise thing to do. Furthermore, note that gum and bone tissue destruction is largely painless. That’s why people tend to take action much later than they should. If you have painless bleeding from the gums while brushing, do not sit idle! Seek a dentist’s advice as soon as possible!
- Gum swelling. Another sign of infection, gum swelling is what eventually leads to receding gums when the disease has advanced to periodontitis.
- Persistent bad breath. Though there are other causes for this symptom, persistent bad breath is strongly associated with periodontitis.
- Pockets between teeth. These are spaces where the tooth’s attachment to the gingival tissue has been destroyed.
- Receding gum line. A receding gum line is the main symptom of periodontitis. Your teeth will have a longer appearance and, in more advanced cases, the roots will begin to be visible.
- Loose teeth. This is a symptom for very late stages of periodontitis.
Risk Factors and Practical Advice
Receding gums and periodontal disease are mainly caused by a combination of internal risk factors, like a weak immune system, some diseases or dental plaque formation. In addition, external risk factors also play a very important role. Addressing all of these in time plays a major role in preventing the appearance of receding gums and periodontal disease.
Internal Risk Factors
- Gum disease, or gingivitis. Gingivitis is the first stage of gum illness, favoring the later appearance of periodontitis. If you have any symptoms of gingivitis, seek advice from a dental care specialist as soon as possible. Gingivitis does not automatically cause receding gums, but is a tell-tale sign that you are at risk to get the condition at some point.
- Diabetes is a risk factor in the appearance of periodontitis and gum disease. If you have diabetes, make sure undertake regular dental checks and keep your eyes open for any red flags regarding the health of your gums.
- Decreased immunity. A weaker immune system will have a harder time combating bacteria in the early stages of gum disease. This can lead to a faster development of receding gums. Depending on the specific condition causing low immunity, visit a specialist to get expert advice on what you should do to prevent the appearance of receding gums.
- Old age. Elderly individuals are more exposed to periodontitis due to the natural recession of gums and tooth decay, which occur with time.
- Hereditary predispositions. Some people have a hereditary predisposition to developing gum disease, for reasons not yet fully understood. If you have a history of dental problems or gum disease in the family, make sure you keep the status of your teeth and gums under close observation.
- Hormonal changes. There appears to be a connection between hormonal changes and a predisposition to gum inflammation and disease. Oral health should be constantly observed during periods of intense hormonal change, such as pregnancy.
External Risk Factors
The internal factors can contribute to our chances of developing receding gums and periodontal disease. But the real culprits behind the very high incidence of periodontitis are our bad habits and our unhealthy lifestyle. A person who is at risk of gum disease but does his/her best to maintain a healthy lifestyle is far less likely to have receding gums that a naturally resilient person with destructivee habits. Some of the main external influencing factors for receding gums are:
- Poor oral hygiene. Receding gums appear first and foremost due to infection caused by plaque and bacteria. The success of such bacteria in the oral environment is only possible if we flagrantly neglect modern oral hygiene standards and practices. If you brush and floss at least twice a day and visit a dentist once every 6 months, your chances of developing receding gums will be drastically reduced.
- Poor diet. In order to properly defend against infection and bacteria, the human body needs a wide variety of substances and compounds, which can only come from a diverse and healthy diet. If you are a fast-food fan and you’re worried about receding gums, consider making some drastic changes to your diet. In addition, dental strength and resilience to decay are also connected to what we eat. Skip junk food and go for green, additive-free products.
- Smoking has a negative impact on gum health. Smoke inhalation fills the mouth with a variety of toxins which affect tissue health. Smoking also stains your teeth and gives your smile an overall unaesthetic aspect.
- Drug abuse. Drug abuse is closely connected to receding gums and periodontal disease and can severely increase the rate at which the disease develops.
Receding Gums Treatment
Periodontitis and receding gums can be treated. It all depends on how much the disease has progressed when treatment begins. The first goal of periodontal treatment is to clean all plaque and bacteria from the teeth, gums and any pockets that might have appeared between the teeth.
A periodontist, i.e. a dentist specialized in periodontal disease, should preferably perform the treatment. Depending on how far the disease has progressed, the treatment can be non-surgical, for mild cases, and surgical, for more severe cases.
Nonsurgical treatments
Dentists use these procedures in less serious cases and are not particularly invasive. Their key goal is to prevent further development of the disease. Some common approaches are:
- Tooth Scaling. This procedure involves a dental care specialist cleaning all plaque and bacteria from your teeth, your gums and from beneath gums. It is very similar to regular tooth cleaning.
- Root Treatment. Dentists use this treatment in cases that are a little more severe due to partial exposure of the root. This treatment involves cleaning and polishing root surfaces to prevent the accumulation of bacteria and plaque.
- Antibiotic Treatment. This treatment is recommended by a dentist in order to help your body fight bacterial infection in your gums. The treatment might include both an oral antibiotic and antibiotic mouthwash.
Surgical treatments
Advanced periodontitis usually requires a more drastic approach. Depending on the specifics of your condition, your dentist could recommend:
- Pocket reduction surgery. This involves the surgeon lifting gum tissue to encourage healing and tissue reconstruction. If the bone is damaged, you might require bone reconstruction beforehand.
- Tissue grafts. This procedure involves taking tissue from another part of your mouth or from a donor and attaching it in places where the gum line has receded. If successful, this can help you cover exposed roots and partially grow back some lost tissue.
- Bone grafts. If the disease has destroyed the bones holding your teeth, periodontists can reconstruct the bone tissue either by collecting bone fragments from elsewhere or by creating synthetic bone. Bone can then grow back and will be able to hold your teeth in place.
These procedures are difficult and extremely costly but are highly successful.
Conclusions
In conclusion, receding gums can be treated, but in serious cases of periodontitis, this will also mean a long recovery period and very high costs. The wisest thing one can do about receding gums is prevention. Good oral hygiene, limiting bad habits and scheduling frequent visits to the dentist can all contribute to preventing gum disease and maintaining a healthy life.



Is so good to see such an in-depth article about receding gums and looking after your teeth. Having good quality dental care which can have a big impact on gum health also has a wider impact on overall body health. Thank you so much for writing, we look forward to visiting again soon.
I’ve recently had to re-think my belief that I took good care of my teeth. I brush (vigourously and thoroughly) twice a day, and floss every day and eat fairly healthily, but had completely overlooked the fact that I drink four or five heavily-sugared coffees a day, which leaves a nice, sugary film on my teeth for hours at a time. Oops!
The coffee (my only vice) will not be given up overnight, and I loathe artificial sweeteners, but I now rinse my mouth after every cup and chew sugar-free gum. I’m upping my calcium too, and now use a remineralising toothpaste. It just goes to show, there’s always more you can do to look after your teeth and gums and it’s a good idea to have a ‘consultation’ with yourself once in a while to check that you’re doing all you can to keep them healthy.